Best Practice Management (PM) Software Buyer's Guide 2026
Emiley Parker
Emiley Parker
Practice management (PM) software is essential to medical practices. Medical practice management (PM) software systems assist physicians and their administrative staff in a variety of ways, including recording patient information, handling charge capture, executing billing operations, generating reports, and scheduling appointments. Practice management (PM) software is also known as POMIS (Physician's Office Management and Medical Information Systems).
Practice Management(PM) software systems can significantly increase a practice's productivity and workflow. They can also increase reimbursements from health insurance companies and other insurance providers.
To have a good understanding of how Practice Management (PM) software works, it is advisable to learn about the different features and functionalities of the software. Before choosing a Practice Management Software, you should check if the software has the following key features:
Automated Billing – A Practice Management software(PM) must offer automated medical billing, including the complete verification of insurance claims and eligibility criteria.
EHR Integration – The PM software must offer practices a choice of incorporating an Electronic Medical Records software (EMR software) system within the software to ensure better record keeping.
Tracking Claims – The top Practice Management (PM) software must allow users to track multiple claims across the revenue cycle.
Coding – The PM software must allow the addition of HCPCS (Healthcare Common Procedure Coding System), CPT codes, as well as ICD (International Classification of Diseases) codes.
Patient Scheduling – The software must provide customized patient scheduling with color-coding capability, which helps indicate appointment duration and time.
Automated Alerts — The top PM software system must be able to send automated electronic reminders to patients via SMS or email. This reduces the chances of no-shows and helps maintain the volume of fixed appointments.
Patient Demographics – The Practice Management (PM) Software should enable the recording and verification of all patient demographics with registered insurance providers.
Reporting – The software must provide practice reporting based on various customizable parameters like billing, scheduling, ICD codes, etc.
Insurance Card Scanner – The PM software must include an insurance card scanner that scans insurance cards and reduces the risk of fraudulent claims.
Security Access – The Practice Management (PM) software must allow administrators to set up individual passwords and different access levels for every user by providing each of them with customized security access.
Electronic Health Records Software (EHR software) represents the electronic method of storing medical records for patients. Using specially designed software, physicians and other medical professionals can store anything ranging from patient demographics to extensive clinical information about patients, such as medical history, social history, lab reports, and more.
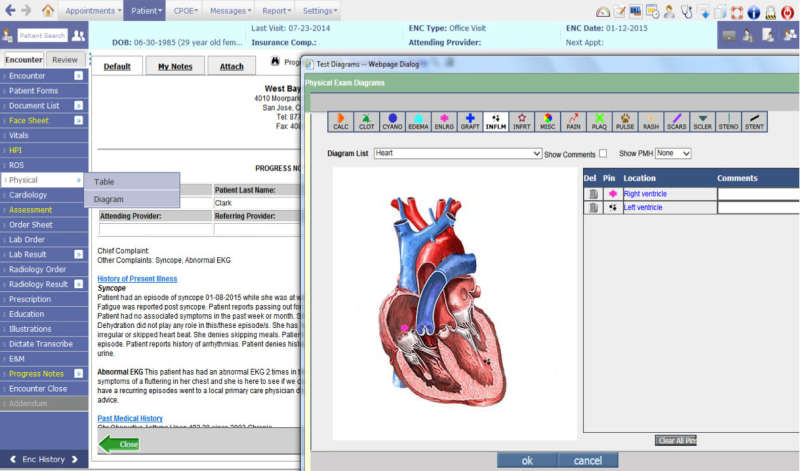
Since all medical providers (MDs, DOs, PAs, NPs, LCSW, OT, etc.) work distinctly based on their background and medical specialty, EHR Software or EMR Software must accommodate the unique style and documentation requirements. Examples of such specialty-specific features include the ability to annotate images and store before/after photos for Pain Management specialists and Dermatology specialists, respectively. Similarly, specialties such as Pediatrics, Oncology, Podiatry, Ophthalmology, Neurology, Nephrology, Dialysis Centers, Rheumatology, and Chiropractic Care require their unique specialty-specific features to simplify adoption.
Since the introduction of the HITECH Act, healthcare IT has undergone a massive transition from the widely recognized Meaningful Use program to what is now known as MACRA, the Medicare EHR Incentive Program. The Meaningful Use program has transformed and now formed part of the four components of the new Merit-Based Incentive Payment System (MIPS), which itself is a fundamental part of MACRA.
For some medical practices, the transition from paper-based records to EMR Software (Electronic Medical Records Software) hasn't been easy. Regardless, realizing that the benefits of utilizing ONC-ATCB Certified EHR Software far outweigh the hassle and challenges associated with it, ensuring a viable future, most practices today have successfully transformed their clinical and administrative operations to EMR Software.
Aside from ensuring tangible financial incentives and profitability, practices converting to EHR / EMR Software have seen the following benefits:
Just like a medical specialty, EHR Software requirements also depend on the size of the medical practice. From solo-provider clinics to large multi-provider, multi-specialty clinics, every practice has unique inherent challenges that need an EMR Software vendor.
A small doctor’s office has a limited number of staff members and a low budget for EMR software compared to a large enterprise such as a hospital. Due to these budgetary constraints, many providers simply choose to employ Free EHR Software or choose an affordable EMR Software vendor with a low fixed monthly fee. Cloud-based access is one such important requirement so that these providers can access patient charts even from home when needed.
These practices usually consist of 5 to 10 medical providers, often belonging to the same medical specialty. Their requirements are more stringent, and their budget is also considerably larger. Aside from specialty-focused requirements (EHR Software by Specialty), these practices also require unique features such as interoperability, dedicated customer support, multi-device support, as well as an extensive reporting functionality to keep an eye on the overall performance of the practice.
Larger group practices generally comprise more than fifteen or, often, twenty medical providers. These practices usually provide medical services that fall under various specialties (Orthopedics, Pain Management, Surgery, Chiropractic Medicine, Family Medicine, etc.). Therefore, these practices require support for multiple users to access the system simultaneously and for the Scheduling software to accommodate multiple locations, providers, and resources, such as dialysis chairs and procedure room allocation. These practices also keep replacing or adding staff members, and need a scalable solution.
EHR software companies, such as Epic, Cerner, AllScripts, NextGen, Athenahealth, IMS by Meditab, eClinicalWorks, Meditech, McKesson, and MEDHOST, typically target and provide solutions for larger corporations, including hospitals, ACOs, PCMHs, IPAs, CINs (Clinically Integrated Networks), and public health departments.
These customers have the most elaborate list of requirements, which are usually documented in the form of an RFI or RFP to assess and shortlist vendors that can meet them. The requirements consist of features like inventory management modules, interface with local labs (LIS), machines, and diagnostic equipment, along with drug dispensing (pharmacy management software) and electronic medication administration records (EMAR), etc.
These entities also require the EHR software to integrate with multiple other software and medical devices.
Since the introduction of Meaningful Use, most healthcare practices have little or no choice but to convert their practice operations to EHR software. However, most providers today select the EHR software that best suits their specific needs and must perform an extensive search to evaluate all available options before they find one that is suitable. Most potential EMR Software buyers in the market today have the following in common:
Although #3 is ideal, every provider and practice workflow is unique, and what works for one provider may not suit another. “One size fits all” simply doesn’t apply in healthcare IT. Software experts and industry specialists are an ideal source of information and advice, and ultimately ensure that the right decision is made.
EMR software includes several types of software based on specific applications or functionalities:
Small doctor offices benefit the most from Cloud-based EMR Software technology since minimal to no upfront cost or maintenance is required, and accessing the EHR Software is possible from any location, given the availability of internet access. This type of EMR software is also device-independent in most cases and can be accessed using devices such as Smartphones (Android & iOS), iPhones, iPads, laptops, and desktop computers.
This is the most significant requirement for most software buyers today as the software must comply with the standards and guidelines set by the Office of the National Coordinator (ONC). The online repository details all software vendors and details related to their respective compliance with the measures set by the ONC (Click here). Software that complies with these standards has undergone rigorous testing and has been confirmed at a benchmark level defined by the federal body. The software testing done during this exercise checks all areas of the EMR Software system, from Patient Portal access to the way the EHR Software communicates with other programs and entities like labs, Pharmacies (via e-Rx), hospitals, HIEs, etc.
With competition rising in healthcare IT, EMR software providing integrated Practice Management software (PM software) as part of their overall software package easily outperforms rivals with standalone EHR Software, including those that may provide specialty-specific EHR software. EMR Software companies with integrated Practice Management Software solutions often tend to provide extensive reporting capabilities to track practice performance and manage business operations better.
Medical practice requires software systems to streamline operations across the board. One such important area is billing for services rendered and communications with insurance companies. Medical Billing Software, therefore, works best when integrated with Electronic Health Records (EHR) software. All clinical documentation seamlessly conforms to the required standard and forms a financial document that can be electronically sent to payers (insurance carriers) to verify and process at their end. This simplifies the operations and ensures all parties are on the same page when it comes to the financial health of the enterprise. Medical billing software helps practices and medical billing managers generate claims, patient statements, verify patient eligibility, and more. This software is ideal for practices that want to handle billing in-house and can integrate with EMR software.
An EMR Software must ensure the security and safety of patient records while ensuring privacy and HIPAA compliance for patient/doctor communication (Patient Portal). This is a paramount concern for physicians, and HIPAA compliance should be guaranteed at all times by the EHR Vendor. Most Vendors today (Epic, Cerner, Athenahealth, AdvancedMD, PrognoCIS, Modernizing Medicine, eClinicalWorks, etc.) are aware of the importance of HIPAA compliance and have taken steps to ensure the safety of patient records security in every section of the EHR Software using advanced tools like data encryption technologies to enhance the security of the EMR software.
One of the decisions medical practices will have to make is whether they want just EMR software or one with integrated Practice Management (PM) software for billing and scheduling. There are advantages to having both together, but there have been cases where some practices only go for one if they had unique requirements that a vendor could not fulfill, or they had already paid a hefty amount for a PM software and weren't looking to replace it yet.
Doctors are not IT professionals, and though some might be tech-savvy, it would be egregious to expect them all to be experts on EHR software. Ease of use is essential to make the transition from paper to electronic smooth, as well as the day-to-day practice to go along without a hitch. If the software is too complicated and hard to understand, it wastes precious time and is needlessly aggravating. Some vendors offer free training while others don't. Make sure you ask for training if your practice needs it.
Not all specialties are created equal, so why must their software be generic? Basic EHR software works well and is good for general practice and most specialties, but doctors have complained about specialty-specific software not being available in the market. The specialty software has built-in recording systems that make specialty practices function efficiently. Only a few vendors provide specialty-specific software, so there aren't many to choose from. But more vendors are cottoning on to the demand, and there should be more options shortly.
Support is a major issue most practices have with their current vendors. A good support team can make small glitches to major roadblocks easy to maneuver, while a bad one will just make things worse. Some vendors provide support as part of the plan you're already paying for, while others charge extra for support. Scout the market, read reviews, or just ask point-blank if there will be a special support team assigned to each practitioner and whether you'll be charged for the service.
There are varying price lists out there; some offer free services, while others charge an arm and a leg for specialty services. Either way, there will be hidden costs that you might get to know about later. Fix your budget and talk to vendors you interview about hidden costs within the contract and whether services such as training and support are free.
Smartphones have changed the dynamics of mobile usage. Handheld devices are easy to carry around and can be used for a number of purposes. Most people are ditching the cumbersome PC for a handheld device. Doctors mostly use iPads or Tablets in the examination room to take down patient symptoms, check history, and note down the prescription, so the vendor must have a mobile application that is synced with all the mobile devices being used in the practice.

Like anything else, the EMR software industry is also subject to constant changes. From new technology to legalities and governing bodies, everything is constantly changing. Here are some of the changes I think it would do well for you to keep track of.
At a healthcare conference, Andy Slavitt, the administrator of the Centers for Medicare & Medicaid Services, declared that Meaningful Use was over. Since then, Meaningful Use has been renamed Promoting Interoperability and has brought along new updates to its core principles.
The program has been overhauled, with the CMS dedicating the program to the exchange of health information and patient data, as well as encouraging medical professionals to implement Certified Electronic Health Records (EHR) software technology.
It's no surprise that more vendors are switching to cloud-based EMR software. Cloud-based EMR software systems can cut down on steep upfront costs that otherwise would be spent on client servers, and they can even be hosted from any device with an internet connection and a web browser, making them a much more convenient option. Research has found that only 25% of practitioners are interested in a web-based EMR Software system, while 50% are willing to have it as an initial model that eventually transitions to a cloud-based.
The EHR software industry is quickly widening its range of practice types to become accessible to a wider range of healthcare services. The number of people who lack the time and knowledge in health IT is increasing each year. This makes optimizing these EMR software solutions more difficult as they must now cater to different needs. Douglas W. Bowerman, MD, predicts we will see a “continued trend towards accessibility” in Electronic Health Records software, both in terms of how we access them – on mobile, for instance – and who can access the EHR software.
Electronic Health Records (EHR) software systems must be inclusive of a wide range of digital capabilities. By working towards better data liquidity, data would be more accessible and therefore increase the EHR footprint, which can be done without compromising on security. Additionally, implementing interoperable electronic health record systems (EHR systems) would also allow better access and exchange of patient information between healthcare organizations.
Currently, Electronic Medical Records software systems are regulated by very lax standards. Due to this, some Electronic Health Records software vendors have had to pay millions of dollars in settlement fees, regarding false claims about meaningful use certifications. Regulations for electronic medical records are becoming far more strict and more transparent to prevent such incidents in the future. Medical billing coders will likely use separate interfaces from physicians as they both require unrelated data, so sharing the same regulations would likely lead to life-threatening miscommunication.
While better patient access is expected of many EHR software systems, the feature has not been completely integrated yet. According to a study in 2019, only 10% of patients (who had access to their records) viewed them. Additionally, of these patients, 63% were encouraged to do so by their respective providers. Vendors of electronic medical records software (EMR software) are updating their systems to be easier to navigate and to better suit patients’ requirements; this also prepares EMR systems for potential future regulatory changes. More health practices are also providing more guidance and raising awareness to encourage more patients to regularly check their health records before appointments.
The growth of your practice can be greatly benefited by boosting patient engagement. One approach can be to make resources and content readily available within patient communities. Another can be to increase patient outreach. Additionally, regular appointment reminders (which can be handled via appointment reminder EMR software) can reduce cancellations and improve patient engagement.
Patients require quick, easy, and secure access to their data so that they can be engaged and informed in their healthcare. The Electronic Medical Records (EMR) software industry is evolving with the latest health IT technology to improve on these points, which will help patients build better trust with their providers. This trend will likely continue for greater health outcomes.
Artificial intelligence (AI) and machine learning have both had major impacts on health IT in recent years. It is likely that as these continue to evolve and change, they will have just as big an impact on EMR software systems. AI and machine learning algorithms can improve Electronic Health Records software by making it more intuitive and efficient, and they can help streamline medical workflows and improve patient outcomes. Applying these technologies to EHR software systems can also enable physicians to provide much more personalized and proactive care by identifying any potential health issues early through analysis of patient data. By providing access and insights into large amounts of patient data, artificial intelligence and machine learning algorithms have the potential to revolutionize clinical research and drug development.