Hospitals in the United States have adopted Electronic Health Records (EHR) software solutions to streamline the care process for patients, digitizing patient records and having all important health data from all providers in one source can improve patient care drastically.
Healthcare institutions and IT professionals must work towards EHR Software interoperability to make way for seamless sharing of patient data across different stakeholders in the healthcare sector which can support care coordination and better communication.
What is EMR Software interoperability?
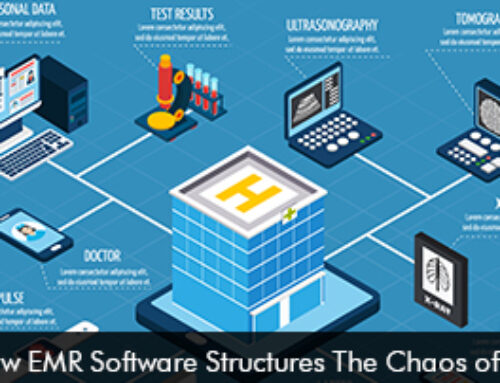
When an EHR software system is interoperable it means that it can smoothly integrate with other software systems to share vital information. With software systems having interoperability options for their users healthcare information can be easily transferred between providers and other systems. The Office of the National Coordinator for Health Information Technology (ONC) revealed that EMR Software solutions must have the following four areas to be integrated seamlessly to be recognized as fully interoperable,
- Software system communication
- Application interaction with clients
- Information processing
- Consumer device integration
Common Features of Interoperable EMR Software
- Interoperability Standard Compliance
- Data Exchange Capabilities
- Integration with External Systems
- Security and Privacy Measures
- Data Standardization
- Scalability
- Mobile Accessibility
By supporting seamless data interchange among healthcare entities, interoperable Electronic Health Records (EHR) software improves care coordination, minimizes medical errors, increases efficiency, and ultimately leads to better patient outcomes.
EHR vendors working for interoperability
Interoperability is a key feature or capability of a top-ranked Electronic Medical Records Software system. Many EHR software vendors are working towards interoperability 3 high-profile EMR Software vendors mainly Epic Systems, athenahealth EMR Software, and Tebra Software are working to make their software products interoperable. This will support data to flow freely and enable patient information to be shared and accessed easily across healthcare IT systems.
Benefits of Interoperability in Healthcare
Helps Protect Patient Data
Medical professionals know how important it is to safeguard sensitive patient information from hackers and these days cybersecurity threats are on the rise. Interoperability in healthcare helps to shield patient data. The employees need not type the same information multiple times as the system accesses the details it requires from the EMR Software system.
Better Care for Patients
When Electronic Health Records Software systems provide interoperability options healthcare providers have quick and easy accessibility to healthcare data. This improves the quality of patient diagnosis and treatment as doctors make accurate decisions with the availability of data. Interoperability also enhances care coordination between providers’ which can make way for better patient care.
Improved Exchange of Data with Other Systems
Interoperable software systems in healthcare help to meet staff and doctors’ needs as information can be transmitted to others. For example, providers can communicate with the patient’s pharmacy and this eliminates the need for handwritten prescriptions. By sending digital prescriptions time can be saved as medication can be dispensed to patients promptly.
Certain Cost Benefits can be realized
Interoperable EHR software systems can help healthcare organizations realize cost benefits quickly as productivity goes up and practices can see more patients in a day. Some processes could be eliminated as clinicians can provide more accurate care after observing that testing has been done previously.
The Value of Interoperability
Interoperability in healthcare is the goal of healthcare professionals as it makes way for improving the patient care process and enhancing efficiency levels. When software systems integrate seamlessly healthcare organizations can save money and witness an improvement in patient outcome levels